Precision Therapy for Lung Cancer Treatment
5 min read
Oncologists are excited about new treatments for lung cancer that are becoming central to patient care – precision therapy. This is a treatment that uses a patient’s tumor DNA to identify the genetic mutations that cause cancer—driver mutations—that can be targeted to kill cancer cells. Using precision therapy for lung cancer treatment, oncologists can develop a customized treatment option for each patient.
Precision therapy provides a valuable addition to our array of standard treatment options, which currently include surgery, radiation, chemotherapy, immunotherapy, or a combination of the aforementioned. The more targets for therapy, the more likely we are to have “the right tool for the right job.”
An Addition to Standard Treatments for Lung Cancer
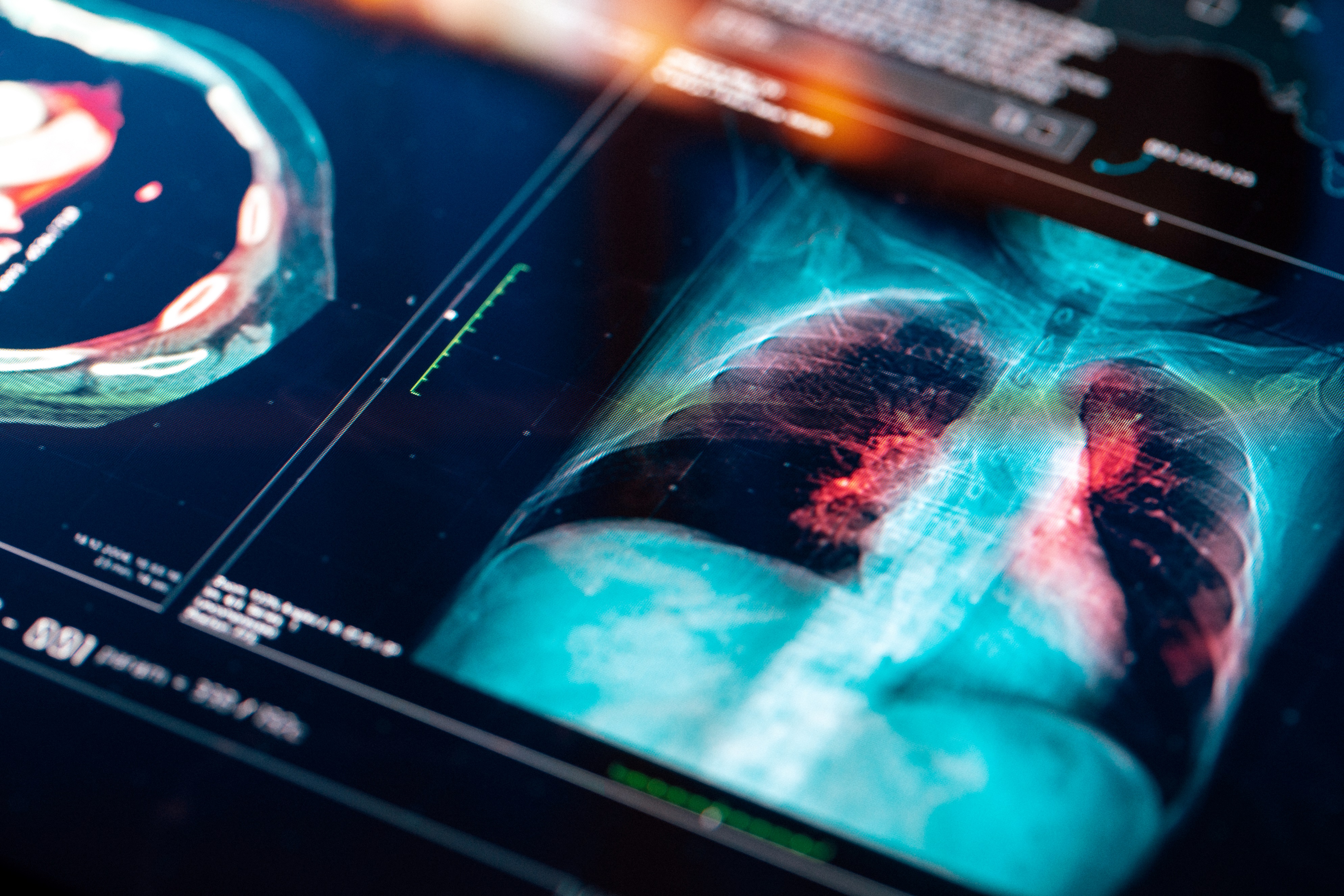
Lung cancer can be identified through imaging and confirmed via biopsy. Imaging modalities include chest X-rays, CT, MRI, and positron emission tomography (PET) scans. Biopsies are often performed via endobronchial ultrasound (EBUS), thoracentesis, or a needle biopsy.
Lung malignancy is broadly categorized into two main categories: small cell (SCLC) or non-small cell cancer (NSCLC). NSCLC is the most common form of the disease. After diagnosis, subsequent lung cancer therapy depends on type (NSCLC vs SCLC) and stage of the disease at diagnosis.
At Rocky Mountain Cancer Centers (RMCC), we offer an array of treatment modalities for lung cancer, however, targeted therapies are now an integral part of treatment. Testing for such “driver mutations” — the genetic mutation/abnormality primarily involved in the tumor generation process — are routinely performed at diagnosis and its corresponding precision therapy is quickly being integrated earlier and earlier in the treatment process.
“Medical advances have added another treatment option for lung cancer – precision therapy,” said Dr. Austin Poole, medical oncologist and hematologist at RMCC. “It’s quickly becoming the new standard of care for patients with NSCLC. Precision therapy targets cancer cells by DNA testing the cancer cells – assessing for mutations that may be eligible for targeted therapy. Precision therapy aims to treat individual cancer patients with therapies specific to their tumor’s genetic (DNA) make-up.”
Precision Therapy for Customized Care
Before oncologists can consider precision therapy, the subtype and stage of disease must be thoroughly evaluated. Each subtype of cancer has a different behavior and genomic (DNA) make-up and, therefore, is treated differently.
At RMCC, we stage lung cancer based on guidelines from the American Joint Committee on Cancer TNM system, which evaluates the size and scope of the principal tumor (T), spread to regional lymph nodes (N), and metastasis (M) to other parts of the body. Precision medicine takes us deeper into the biology and characteristics of each specific tumor.
What It Means for Patients
Once physicians identify these driver mutations, we target them with specific treatments known to kill cancer cells. For example, the first driver mutation treatment researchers identified in NSCLC were epidermal growth factor receptor (EGFR) mutations. These mutations are sensitive to EGFR tyrosine kinase inhibitors. Since then, scientists have identified other biomarkers and corresponding treatments with the US Food and Drug Administration (FDA) approval of their corresponding targeted therapy. To date, there are seven biomarkers for NSCLC with approved FDA treatments and more currently under investigation in clinical trials.
Testing for specific targets is carried out by something called next-generation sequencing. This allows oncologists to customize treatment options – whether that be through standard of care options or via investigational treatment options on a clinical trial.
“Of interest, we are now able to look for these ‘driver mutations’ through blood samples – assessing circulating tumor cells,” Dr. Poole said. “This provides a rapid assessment, allowing treatment to be initiated more quickly. This is a way to identify biomarkers in a more non-invasive way.”
Lung Cancer: Still a Societal Burden
Lung cancer is the second most common cancer in both men and women and accounts for nearly 25% of cancer deaths in the U.S. Patients diagnosed with lung cancer are usually older; the average age at diagnosis is around 70 years.
Of note, many of those diagnosed later in the disease process had known risk factors and could have, given the proper information and screenings, received diagnosis and treatment at an earlier stage when the cancer is more curable.
Lung cancer can occur in people younger than 45 years of age, but it is rare.
“The leading risk factor for lung cancer is smoking,” Dr. Poole said. “Other considerations are inhalation or ingestion of toxic chemicals, including silica and asbestos, and radon exposure.”
Other factors that can predispose someone to lung cancer include exposure to drinking water contaminated with arsenic, prolonged inhalation of chemicals such as diesel exhaust, previous history of chest radiation therapy (e.g. for breast cancer), and family history. Non smoking-related cases make up approximately 20% of diagnoses but these non smoking-related cancers tend to be enriched in those genetic alterations that lend themselves to targeted therapy, over and above those alterations seen in smoking-related disease.
Symptoms to Watch For
Symptoms of lung cancer vary depending on the patient and cancer stage. Generally, signs of lung cancer center around symptoms in the chest area and constitutional symptoms such as:
 Swollen lymph nodes in the chest seen on imaging
Swollen lymph nodes in the chest seen on imaging- Persistent coughing with or without blood in sputum
- Chest pain
- Wheezing
- Shortness of breath
- Unexplained weight loss
- Prolonged unexplained fatigue
According to Dr. Poole, symptoms tend to be vague and often overlap with other health conditions, making screening that much more important.
“We often diagnose lung cancer at later stages due to this misattribution of symptoms,” he said. “This is why it’s important to take a thorough medical history – including any potential occupational exposures and past or current smoking habits. The U.S. Preventive Services Task Force (USPSTF) focuses on lung cancer screening based on smoking history, but we know lung cancer can develop from causes other than tobacco use.”
Unfortunately, not all people who smoke or used to smoke know about screening recommendations.
USPSTF Screening Guidance
The USPSTF recommends screening for lung cancer for a subset of the general population with a smoking history. Yearly screening by low-dose tomography (LDCT) is recommended for individuals meeting the following criteria:
Age between 50 and 80, and
- Currently smoke or have quit in the past 15 years
- Have a 20 pack-year or more smoking history (packs per day times years of smoking)
RMCC depends on community providers to educate patients about risk factors, explain screening options, and increase awareness of signs that might point to lung cancer.
Rocky Mountain Cancer Centers is proud to offer the most up-to-date advancement in cancer treatment through participating in over 500 clinical trials at any given time. We have a team of experts focused on precision therapy for lung cancer treatment and welcome referrals of patients diagnosed with lung cancer. Visit RockyMountainCancerCenters.com/lung-cancer for more information.