Saving Lives Through Routine
Cancer Screening
Cancer screening is the process of checking for cancer when there are no symptoms. Screenings are available for several types of cancer. Keep reading to learn more. Then talk to your doctor about your personal risk level and the right timing for your cancer screenings.

Screening Recommendations by Type of Cancer
There are standard screening guidelines for several types of cancer based on people who are at average risk for cancer. There are also recommendations for those who are at a higher risk. Be sure you know your risk category and talk to your doctor about when to start screenings for various types of cancer.
Click a cancer type below to learn more about how it's screened.
How to Get Screened for Cancer
Most screening tests are requested by your primary care doctor or gynecologist. Talk to your doctor about the various screenings you may need as you approach 40 to see what’s right for you based on your personal risk factors.
If you don’t have a doctor, there are things you can do and places you can call to find out how to get the screening tests you need. Call a local hospital, medical clinic, or health department and explain your situation, they might be able to guide you to a facility that does the screening test or to a clinic or doctor that can help.
Don't put it off.
Schedule your cancer screenings!
Cancer Screening Guidelines
Types of Tests Used for Cancer Screenings
Screening for cancer is typically covered by insurance. Each screening process is different and can include some of these testing procedures.
Examinations
Exam of specific areas of the body used to help detect abnormalities:
- Clinical breast examination
- Digital rectal examination for prostate and rectal cancers
Imaging Tests
Tests that produce pictures of areas within the body:
- X-ray, CT, MRI
- Mammography for breast cancer
- Ultrasound
Laboratory Tests
Tests that check; blood, urine, and other body fluids and tissues
- Pap test for cervical cancer
- Fecal occult blood test for colorectal cancer
Visual
Visual examinations by a health care professional
- Colonoscopy for colorectal cancer
- Skin examination to look for any signs of skin cancer
Importance of Cancer Screenings
Breast Cancer Screening
Most women won't experience symptoms of breast cancer, especially in the early stages. That's why screening is so important! It's good to know how your breasts normally look and feel so you can report any changes to a health-care provider right away.
Some women – because of their family history, a genetic tendency, or certain other factors – should be screened with MRIs along with mammograms. (The number of women who fall into this category is very small.) The American Cancer Society recommends against MRI screening for women whose lifetime risk of breast cancer is less than 15%.
American College of Radiology (ACR) and Society of Breast Imaging (SBI) now recommend that ALL women should be evaluated for breast cancer risk no later than age 30 (review personal and family history and complete risk-assessment).
Learn more about breast cancer screening and watch our video to see if it’s right for you.
Talk to your gynecologist or primary care physician at your annual exam about the right breast cancer screening schedule for you.
Be screened with a mammogram annually.
Continue with mammograms if your overall health is good, and you have a life expectancy of 10 or more years.
Women who are high risk for breast cancer should get a breast MRI and a mammogram annually, typically starting 10 years prior to earliest breast cancer diagnosis in the family.
Risk factors include:
- A lifetime risk of breast cancer of about 20% or greater, according to risk assessment tools that are based mainly on family history (i.e. Tyrer Cuzick)
- A known BRCA1 or BRCA2 gene mutation (based on having had genetic testing) or other genetic predisposition for breast cancer
- A first-degree relative (parent, brother, sister, or child) with BRCA1 or BRCA2 gene mutation, but you have not had genetic testing yourself
- Previous radiation therapy to the chest when you were between the ages of 10 and 30 years

Breast Cancer Screening: What's Right for You?
Learn more about breast cancer and how it's screened. If you're in the age range for breast cancer screening, be sure you have a plan in place. Talk to your doctor about what's right for you.

Related Reading: A Guide to Your First Mammogram
Cervical Cancer Screening
For many women, a diagnosis of cervical cancer comes without warning since in its earliest stages there may be no signs or symptoms that something is wrong. Doctors recommend that women help reduce their risk of cervical cancer by having regular Pap tests. A Pap test (sometimes called Pap smear or cervical smear) is a simple test used to look at cervical cells. Pap tests can find cervical cancer or abnormal cells that can lead to cervical cancer.
No screening needed.
Cytology (PAP) once every three years.
Women should have an HPV test every five years, a PAP every three years, or an HPV/PAP co-test every five years.
No screening needed if a series of prior tests were normal.
Colorectal Cancer Screening
Screening for colorectal cancer is important because symptoms rarely appear until the tumor has grown considerably.
Risk factors for colorectal cancer include your age, race, personal history of polyps and your family history of polyps and colorectal cancer. People of average risk should start talking to their doctors about colorectal screening at age 45. If you're at high risk screening might start sooner.
Some risk factors for developing colorectal cancer can be controlled such as:

Screening for colorectal cancer can be done in a few ways based on your risk level.
Stool-based Tests
-
Highly sensitive fecal immunochemical test (FIT) every year
-
Highly sensitive guaiac-based fecal occult blood test (gFOBT) every year
-
Multi-targeted stool DNA test (mt-sDNA) every three years
Visual (Structural) Exams of the Colon and Rectum
-
Colonoscopy every 10 years for average risk; more frequent based on personal and family history or if pathology identified
-
CT colonography (virtual colonoscopy) every five years; more frequently if pathology identified
-
Flexible sigmoidoscopy (FSIG) every five years; more frequently if pathology identified
Learn more about colorectal cancer screening.
Talk to your primary care physician at your annual exam about the right colorectal cancer screening schedule for you.
Testing may be recommended if you have a higher-than-average risk of colon cancer.
People at average risk (are in good health and with a life expectancy of more than 10 years) should have regular colorectal cancer screenings.
The decision to be screened should be based on your preference, life expectancy, overall health, and prior screening history.
Colorectal cancer screenings are no longer required.
People who are at an increased or high risk for colorectal cancer might need screening before the age of 45, be screened more often, and/or get specific tests.
Risk factors include:
- A personal history or a strong family history of colorectal cancer or certain types of polyps
- A personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease)
- A known family history of a hereditary colorectal cancer syndrome such as familial adenomatous polyposis (FAP) or Lynch syndrome (also known as hereditary non-polyposis colon cancer or HNPCC)
- A personal history of radiation to the abdomen (belly) or pelvic area to retreat a prior cancer
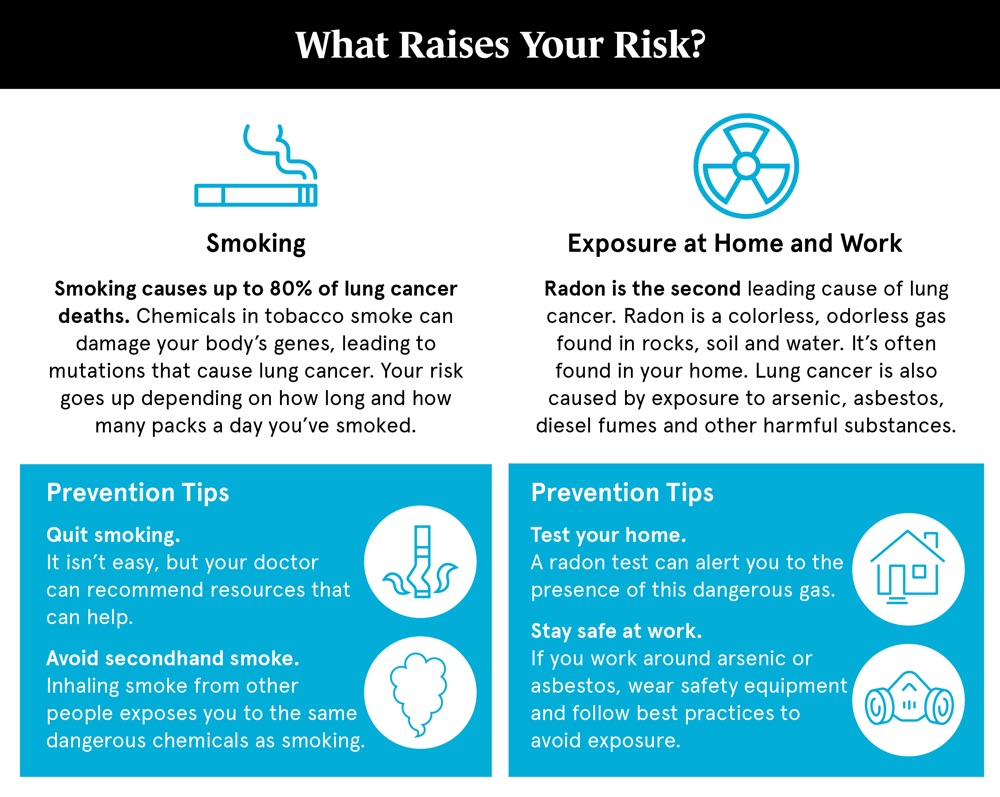
Lung Cancer Screening
A lung cancer screening test is now available for those who qualify based on their history of smoking. A low-dose chest CT scan is performed to see if there are early signs of cancer developing in the lungs.
Age 50-80: An annual lung cancer screening with a low-dose CT scan is recommended if you are:
- In fairly good health
- A current or former smoker
- Have at least a 20 pack-year smoking history
Learn more about lung cancer screening and watch our video to see if it’s right for you.
Talk to your primary care physician at your annual exam about the right lung cancer screening schedule for you.
Related Reading

When Should You Start Colon Cancer Screenings?
Screening is important because it can prevent colorectal cancer by finding anything abnormal and treating it promptly before it develops into cancer.
Can I Be Screened for Lung Cancer?
Pancreatic Cancer Screening
People who are considered high risk should have an MRI/MRCP and/or endoscopic ultrasound annually, starting at age 50 (or 10 years prior to the earliest diagnosis in the family).
Risk factors include:
- Certain gene mutations such as ATM, BRCA1, BRCA2, PALB2 mutation, and others
- Family history of pancreatic cancer in two or more first-degree relatives
- Family history of pancreatic cancer in three or more first and/or second-degree relatives
Prostate Cancer Screening
Starting at age 50, men should talk to a health care provider about the pros and cons of prostate cancer testing so they can decide if testing is the right choice for them.
If you are African American or have a father or brother who had prostate cancer before age 65, you should have this talk with a health care provider starting at age 40.
If you decide to be tested, you should get a PSA blood test with or without a rectal exam. How often you’re tested will depend on your PSA level.
Learn more about prostate cancer screening and watch our video to see if it’s right for you.
Talk to your urologist or primary care physician at your annual exam about the right prostate cancer screening schedule for you.
No screening is needed unless you are considered high-risk.
Screening with prostate-specific antigen (PSA) test should be considered for people with average risk. The decision to screen with PSA should be based on patient preference, family history, and current health.
Screenings are no longer required.
Screening with a PSA should be considered for high-risk populations and African Americans with a positive family history starting at age 40.
Risk factors include:
- Men with a first-degree relative (father or brother) who had prostate cancer at an early age (younger than age 65)
- Men with a genetic predisposition for prostate cancer (BRCA1/2 positive or other genes)
What are Prostate Cancer Risk Factors?
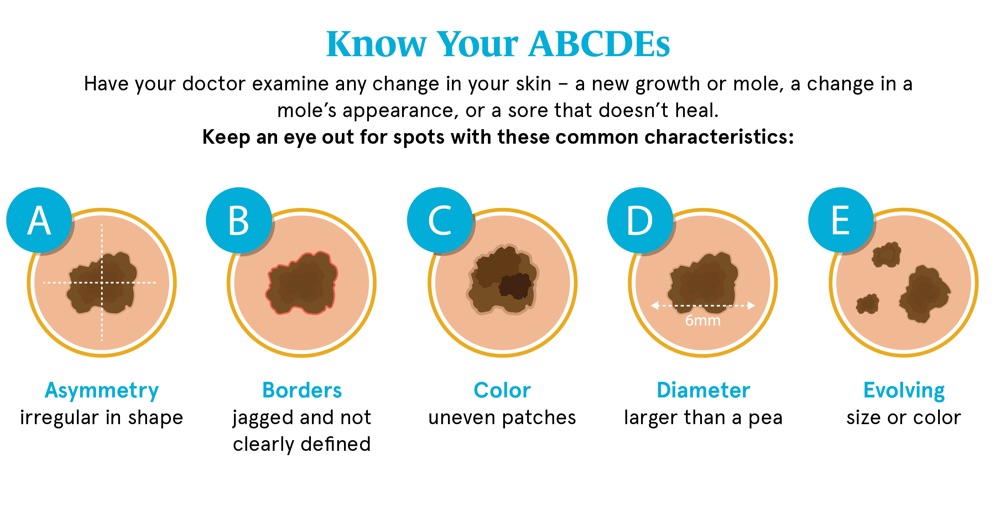
Skin Cancer Screening
Periodic skin examinations are the key to diagnosing skin cancer at its earliest stage, when it is most easily cured.
If you’re at increased risk for skin cancer, you may need an annual skin cancer screening exam. You may be at increased risk if you have:
- Red or blond hair, fair skin, freckles and blue or light-colored eyes
- More than 50 moles
- History of frequent or intense sun exposure
- One or more blistering sunburns
- Family history of melanoma
- Personal history of basal cell and/or squamous cell skin cancers
Even if you aren’t at increased risk, it’s a good idea to keep an eye on your skin. If you notice an irregular mole or spot, schedule an appointment with your dermatologist for a diagnostic exam.
Learn more about skin cancer screening and watch our video to see if it’s right for you.
Talk to your dermatologist or primary care physician at your annual exam about the right skin cancer screening schedule for you.