Chemotherapy Benefits in Invasive Lobular Carcinoma
5 min read

Following an invasive lobular carcinoma (ILC) diagnosis, there are different treatment options available to your patient. Choosing the right one for your patient depends on the stage, the aggressiveness of the cancer, and the patient’s health and preferences. Treatment options may include surgery and additional adjuvant therapy, including radiation, hormone therapy, and chemotherapy.
What Is Invasive Lobular Carcinoma?
ILC originates in the milk-producing glands and can spread to other parts of the body if left untreated. It is the second most common form of invasive breast cancer, accounting for 5% to 15% of all invasive breast cancers with the most common being invasive ductal carcinoma (IDC). Invasive lobular carcinoma incidence rates have markedly increased over the past two decades, likely due to diagnostic advances.
 “ILC is associated with risk factors related to the use of prolonged and increased exposure to hormone replacement therapy, particularly progesterone,” said Dr. Praveena Solipuram, MD, medical oncologist and hematologist at RMCC. “In addition, other hormone-related risk factors, such as low parity, late menopause, late age at first birth, and earlier menarche are associated with a higher incidence of ILC.”
“ILC is associated with risk factors related to the use of prolonged and increased exposure to hormone replacement therapy, particularly progesterone,” said Dr. Praveena Solipuram, MD, medical oncologist and hematologist at RMCC. “In addition, other hormone-related risk factors, such as low parity, late menopause, late age at first birth, and earlier menarche are associated with a higher incidence of ILC.”
Additional risk factors that make some people more prone to developing ILC include:
- Older age. Your risk of breast cancer increases as you age. Women with invasive lobular carcinoma tend to be a few years older than women diagnosed with other types of breast cancer.
- Female. While males can develop breast cancer, women are more likely to.
- Postmenopausal hormone use. The use of estrogen and progesterone during and after menopause increases the risk of ILC.
- Previous diagnosis of lobular carcinoma in situ (LCIS). LCIS increases the risk of developing invasive cancer in either breast.
- Family history of breast or ovarian cancer. Women with a first-degree relative (mother, sister, or daughter) have an increased risk of invasive lobular carcinoma.
- Inherited genetic cancer syndromes. Women with a rare inherited condition called hereditary diffuse gastric cancer syndrome have an increased risk of both stomach (gastric) cancer and invasive lobular carcinoma.
Diagnosis of Invasive Lobular Carcinoma
Diagnosis of ILC can be particularly challenging because it’s hard to see on imaging tests. “In addition, ILC hasn't been studied as much as invasive ductal cancer,” said Dr. Solipuram, “and in the early stages of invasive lobular carcinoma, there may not be any noticeable signs since this type of breast cancer is less likely to cause a firm or distinct breast lump.”
As time goes on, ILC patients may experience:
- An area of thickening or swelling in part of the breast
- A change in texture or appearance of the skin over the breast (e.g., dimpling or thickening)
- A newly inverted nipple
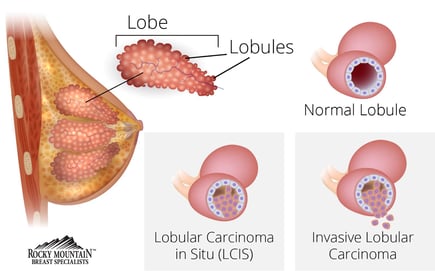
Diagnosis of ILC is difficult due to distinctive biological hallmarks, including loss of cell adhesion molecule E-cadherin, which leads to cells with a discohesive morphology and proliferation into single-file strands.
As a result of the biological hallmarks, diagnosis by physical exam of ILC is challenging since patients often present with limited clinical signs and do not always have a breast lump. Patients may report skin thickening or dimpling without a palpable breast lump.
While mammography is considered the “gold standard” for diagnosing breast cancer, ILC is challenging to detect due to the infiltrative tumor growth pattern.
“ILC is difficult to detect on a mammogram because ILC cells grow linearly compared to the clumps or masses other breast cancer cells form,” Dr. Solipuram said.
The sensitivity in detecting ILC with a mammogram is between 57% and 81%, with 8% to 24% false-positive rates. Using ultrasound in conjunction with a mammogram and physical exam yields a much better detection rate of ILC with a sensitivity of 68% to 98%.
Due to the nature of ILC, MRI is used in the screening of high-risk breast cancers and comparing mammogram and ultrasound findings. MRI has a sensitivity of 93% in detecting ILC. Although the use of MRI provides additional diagnostic information that can be missed in standard imaging, this tool should be used in conjunction with other imaging tools to assess patients with ILC accurately.
Chemotherapy as a Treatment Option
Once ILC is diagnosed, it’s imperative to start treatment right away. Because it’s possible for ILC to spread to the bloodstream or lymph nodes, time is crucial in preventing metastatic breast cancer. Treatment of ILC isn’t a straightforward process and typically involves more than one treatment modality. Generally, treatment for ILC requires surgery to remove cancer cells in addition to adjuvant treatment such as radiation or chemotherapy.
Since most ILCs are hormone receptor-positive, most treatments are aimed at endocrine-based therapy. Research shows that ILC often has a good prognosis since the cancer cells are generally low grade and respond well to hormone treatment. Due to the biological characteristics of ILC, it is considered less responsive to chemotherapy than other types of breast cancer, resulting in lower rates of complete pathological response.
While treatment of ILC with chemotherapy neoadjuvant therapy is less responsive, there are benefits of using chemotherapy in ILC, such as relieving tumor burden to allow breast-conserving surgery to be performed and improving quality of life. Adjuvant treatments after surgery with chemotherapy are often not performed since the disease is slow-growing and usually responds positively to hormone treatment alone. Despite the report of chemotherapy having less responsiveness in ILC, a subset of ILC patients at high risk of recurring and progressing disease may benefit from the use of chemotherapy.
The MINDACT clinical trial identified a subset of ILC patients who survived without the disease spreading or a recurrence of the disease at five years was comparable to high-risk ILCs and IDCs classified by MammaPrint. The 70-gene signature test identified patients with a genetic makeup that puts them at high risk of recurring cancer when treated alone with hormone therapy. This subset of patients may benefit from additional adjuvant treatment with chemotherapy.
Additionally, lobular cancer responsiveness to chemotherapy has been shown to be equivalent to ductal cancer with similar profiles. Data has shown a connection in chemotherapy treatment and survival benefit for patients with an intermediate or high-level oncotype recurrence score. Research conducted on the responsiveness of lobular cancer to chemotherapy found a notable five-year survival outcome when chemotherapy is used for high-RS patients who have ILC.
What does all this emerging data regarding chemotherapy and invasive lobular carcinoma mean? This new data suggests that although most patients with ILC are not chemosensitive, there is a subset of high-risk ILC patients that benefit from chemotherapy to increase their survival rate.
“Our ultimate goal is to improve survival outcomes in ILC patients with a high oncotype recurrence score,” said Dr. Solipuram. “The use of adjuvant chemotherapy seems to provide an overall survival benefit as compared to not using chemotherapy in patients with a high-recurrence subtype. We’re committed to exploring this treatment option and providing the most up-to-date cancer treatments at Rocky Mountain Cancer Centers.”
RMCC focuses on an independent, community-based model of cancer care that is patient-centered and evidence-based. Our expert multidisciplinary team offers expertise in all areas of breast care. We welcome referrals of patients with ILC or any other form of breast cancer.
Visit RockyMountainCancerCenters.com/Breast-Cancer/Breast-Specialists for more information on our breast care clinics in Colorado.